Tesla has officially launched the Model Y in India, opening bookings nationwide through its official website. Indian consumers can now reserve this luxury electric SUV by paying an initial amount of ₹22,220. But before you jump in, here’s everything you need to know about the car, the booking process, and cancellation policies.
Tesla Enters Indian Market with Model Y
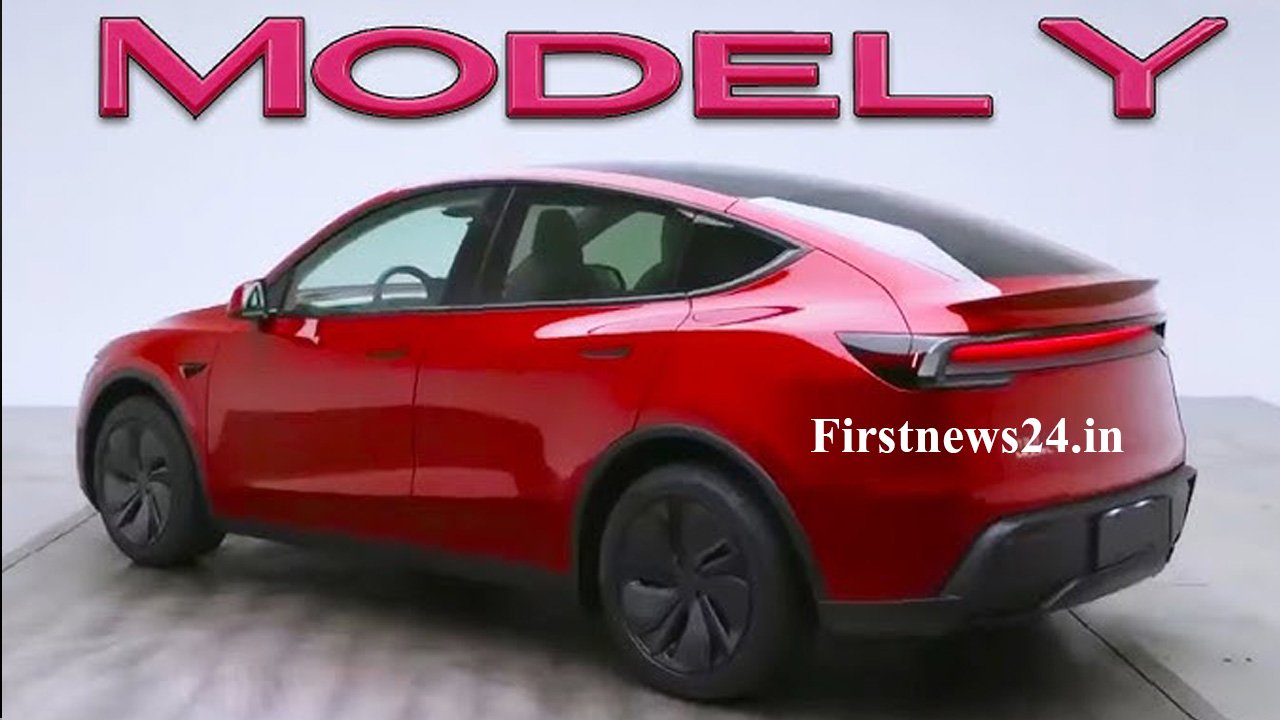
The long wait is finally over—Tesla has made its debut in India with the Model Y, a premium electric crossover SUV. With a starting ex-showroom price of ₹59.89 lakh, the Model Y blends performance, innovation, and sustainability. The vehicle comes in two variants: Rear-Wheel Drive (RWD) and Long Range RWD.
OnePlus 13R 5G Now Available at a Discount on Amazon: ₹3,000 Bank Offer, Exchange Bonus & More
Performance and Range
-
Rear-Wheel Drive (RWD):
Offers a WLTP-certified range of 500 km and accelerates from 0–100 km/h in just 5.9 seconds. -
Long Range RWD:
Delivers an extended range of 622 km and completes the 0–100 km/h sprint in 5.6 seconds with a top speed of 201 km/h.

Design & Features
The Model Y stands out with:
-
Sleek 19-inch Crossflow alloy wheels
-
A minimalist, fully digital interior
-
Choice of six exterior colors
-
Access to Tesla’s advanced Full Self-Driving (FSD) system, available as an add-on for ₹6 lakh.
Priority Delivery in Metro Cities
Tesla plans to roll out deliveries in phases. In Phase 1, customers in Mumbai, Pune, Delhi, and Gurugram will receive their vehicles first. Other cities will follow in Phase 2.
Sony Xperia 1 VII vs Huawei’s 2025 Flagships: Who’s Leading the Future of Smartphones?
Booking Details: What You Should Know
Interested buyers can reserve the Model Y through Tesla’s official website with a two-step payment process:
-
₹22,220 (non-refundable) at the time of booking
-
₹3,00,000 (also non-refundable) within 7 days of booking
Both amounts include TCS (Tax Collected at Source). Tesla emphasizes that this is a non-refundable process, so potential buyers should proceed with caution.
Is It Worth It?
Tesla’s entry into India is a major milestone for the country’s electric vehicle market. The Model Y is more than just a car—it represents a vision of a cleaner, smarter future. If you’re ready to make the switch to electric and want a car that combines tech, luxury, and performance, this could be the right time.
People Also Ask
Is Tesla Model Y available in India now?
Yes, Tesla Model Y is now available for booking in India via the official Tesla website. Deliveries will begin in select metro cities in Phase 1.
How much does it cost to book Tesla Model Y in India?
To book the Model Y, you’ll need to pay ₹22,220 initially, followed by ₹3,00,000 within 7 days—both are non-refundable and include TCS.
What is the range of Tesla Model Y in India?
The Rear-Wheel Drive variant offers up to 500 km, while the Long Range RWD delivers up to 622 km on a single charge.
Where will Tesla cars be delivered first in India?
Tesla will prioritize deliveries in Mumbai, Pune, Delhi, and Gurugram as part of its first phase.
Can the booking amount be refunded?
No. Both the initial ₹22,220 and the second installment of ₹3,00,000 are non-refundable, even if the booking is cancelled.